Evidence has shown that many with Chronic Low Back Pain (CLBP) experience sleep disturbance, reduced sleep duration and sleep quality, increased time taken to fall asleep, poor day-time function and greater sleep dissatisfaction and distress (Kelly et al, 2011). Sleep is however, vital for tissue regeneration, growth and energy conservation so someone with CLBP will most likely benefit physically and mentally from a good nights sleep.
Evidence has shown that many with Chronic Low Back Pain (CLBP) experience sleep disturbance, reduced sleep duration and sleep quality, increased time taken to fall asleep, poor day-time function and greater sleep dissatisfaction and distress (Kelly et al, 2011). Sleep is however, vital for tissue regeneration, growth and energy conservation so someone with CLBP will most likely benefit physically and mentally from a good nights sleep.
Chronic pain and sleep disturbance have a reciprocal relationship and are often found together. Pain can limit sleep duration and sleep deprivation and poor quality sleep can decrease pain thresholds and limit the mental capacity to manage pain. With more than 50% of people with CLBP experiencing difficulty with sleep, it’s unclear as to whether sleep disturbance is a cause or an effect of chronic pain (Tang et al, 2007; Marin et al, 2006).
Contents
Why do I have more pain at night?
As you will already have guessed, chronic back pain is complicated and there could be a combination of reasons why you are experiencing more pain at night.
Stress hormone levels vary across a 24 hour period and at night they are at their lowest. It could be that this change in hormones allows pain signals to the brain to increase, it could also be that it’s easier to be more aware of the pain as you lie in quiet trying to sleep.
There are also mechanical factors that could be exacerbating your pain as you lie down. Blood supply alters at night as does the mechanical load on your spine.
How should I sleep with lower back pain?
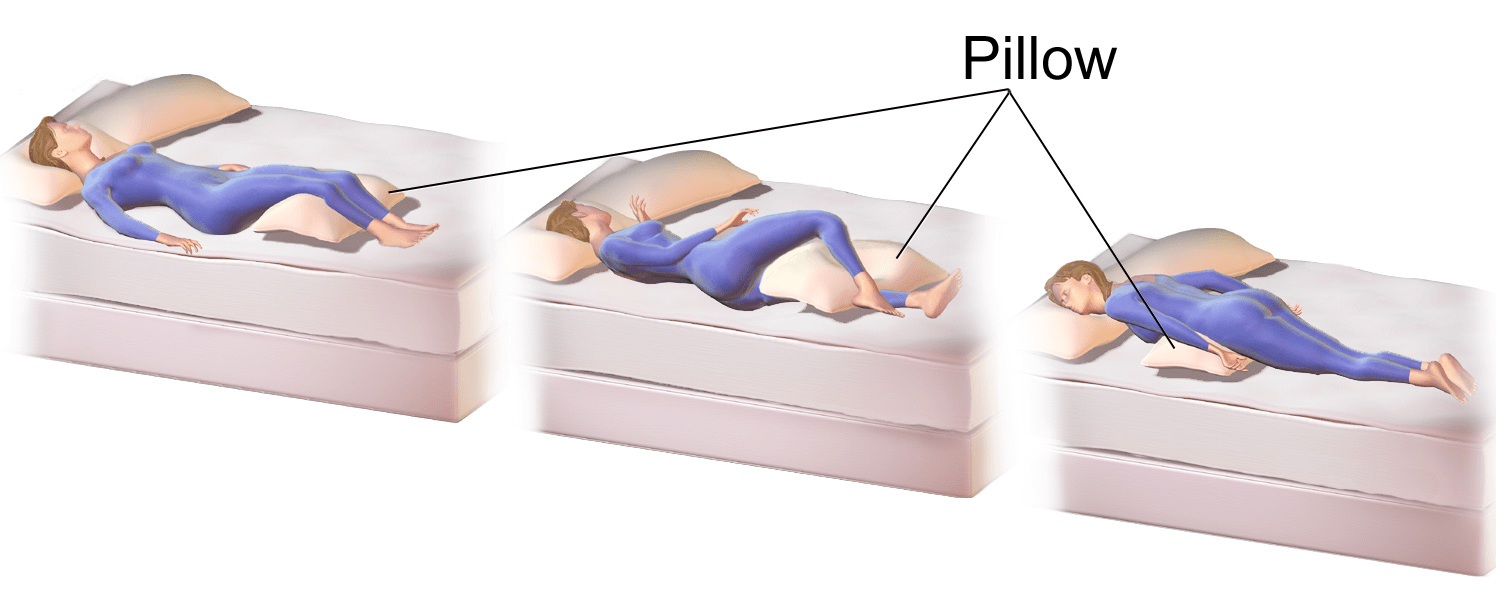
Many of our participants already have sleep routines and positions that work for them and others take the opportunity in our programme to try out new techniques. One of the most recommended techniques is to sleep with a pillow between your legs when sleeping on your side. This and more ideas can be found here.
What else can I try?
There are a range of techniques for improving sleep quality and duration. CBT has been shown to have a positive effect and is about recognising, challenging and changing the way that we think and act in regard to our sleep. You can read more about it here.
What should I do in the morning?
When we lay down to sleep at night, the spine is unloaded, so the intervertebral discs relax and fully hydrate. This increased hydration status builds tension within the discs, and makes the spine stiffer overall (McGill, 2004). In becoming stiffer more stress is placed on the ligaments and discs than the soft tissue structures that typically protect them.
This means that we need to give our bodies time to readjust when we get up in the morning. As we move around first thing we should aim to stand upright as much as possible to allow the hydration status of the discs to decrease. The majority of the good work is done within 30-60 minutes but for this reason those with back pain should avoid doing their core exercises first thing in the morning.
References
Kelly, G. A., Blake, C., Power, C. K., O’keeffe, D., & Fullen, B. M. (2011). The association between chronic low back pain and sleep: a systematic review. The Clinical Journal of Pain, 27(2), 169-181.
Marin, R., Cyhan, T., & Miklos, W. (2006). Sleep disturbance in patients with chronic low back pain. American Journal of Physical Medicine & Rehabilitation, 85(5), 430-435.
McGill, S. M. (2013). Ultimate Back Fitness and Performance, Backfitpro Inc., Waterloo, Canada.
Sezgin, M., Hasanefendioğlu, E. Z., Sungur, M. A., Incel, N. A., Çimen, Ö. B., Kanık, A., & Şahin, G. (2015). Sleep quality in patients with chronic low back pain: A cross-sectional study assesing its relations with pain, functional status and quality of life. Journal of Back and Musculoskeletal Rehabilitation, 28(3), 433-441.
Tang, N. K., Wright, K. J., & Salkovskis, P. M. (2007). Prevalence and correlates of clinical insomnia co‐occurring with chronic back pain. Journal of Sleep Research, 16(1), 85-95.