Saturday 26th June 2021 – Tuesday 27th July
Hours: 8 (2 x 1 hours sessions over 4 weeks)
Patient presentation pre:
- QASLS
- Affected limb 4
- Unaffected limb 2
- Quadricep LSI
- 87.5% with the affected limb showing weakness
- H:Q
- 100% both legs but affected limb weaker than unaffected
- ACL-RSI
- 50
- IKDC
- 80
- 28-year-old female, 18 months post-operative from an anterior cruciate ligament reconstruction (ACL-r). Their goal is to fully return to hockey and would like to alter their current weight training programme to reflect this. In order to return to hockey, the client wants to improve the stability of their knee and gain the confidence needed to trust that their knee can perform at a sporting level again.
Reflection Model
- Gibbs Reflective Cycle 1988
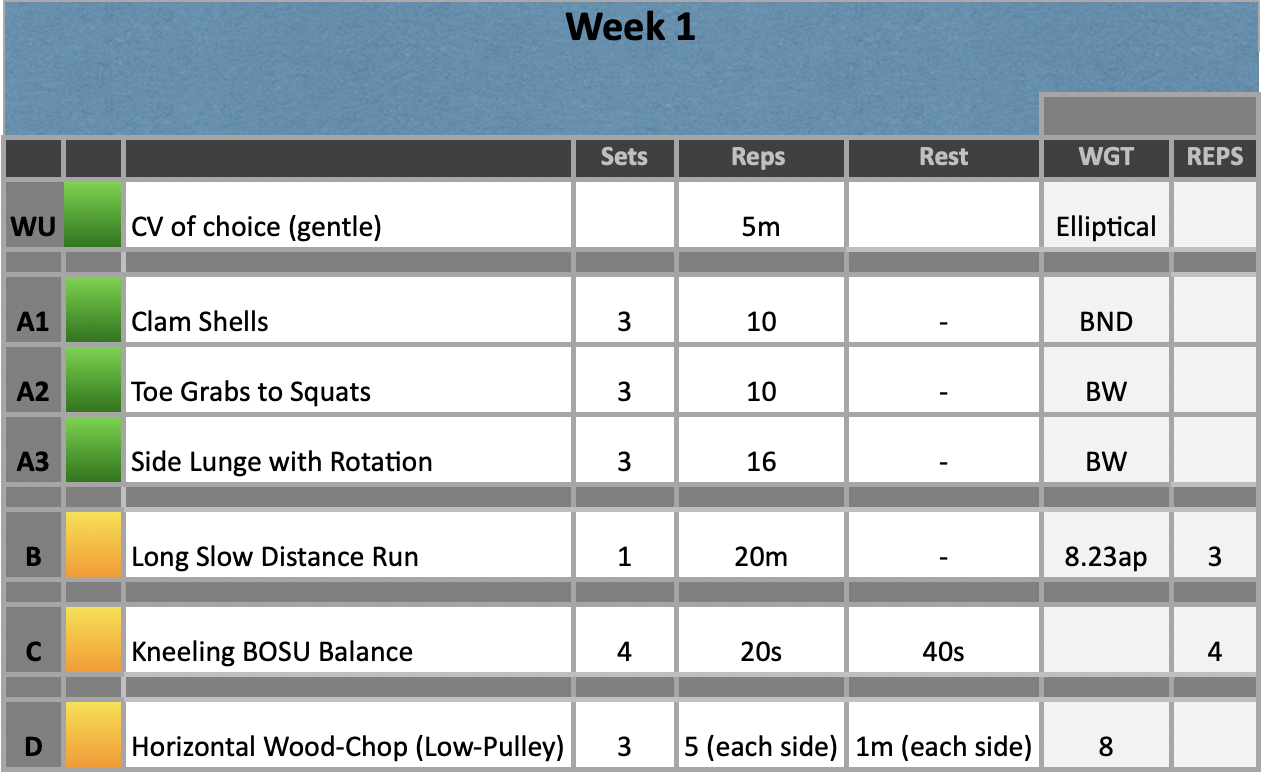
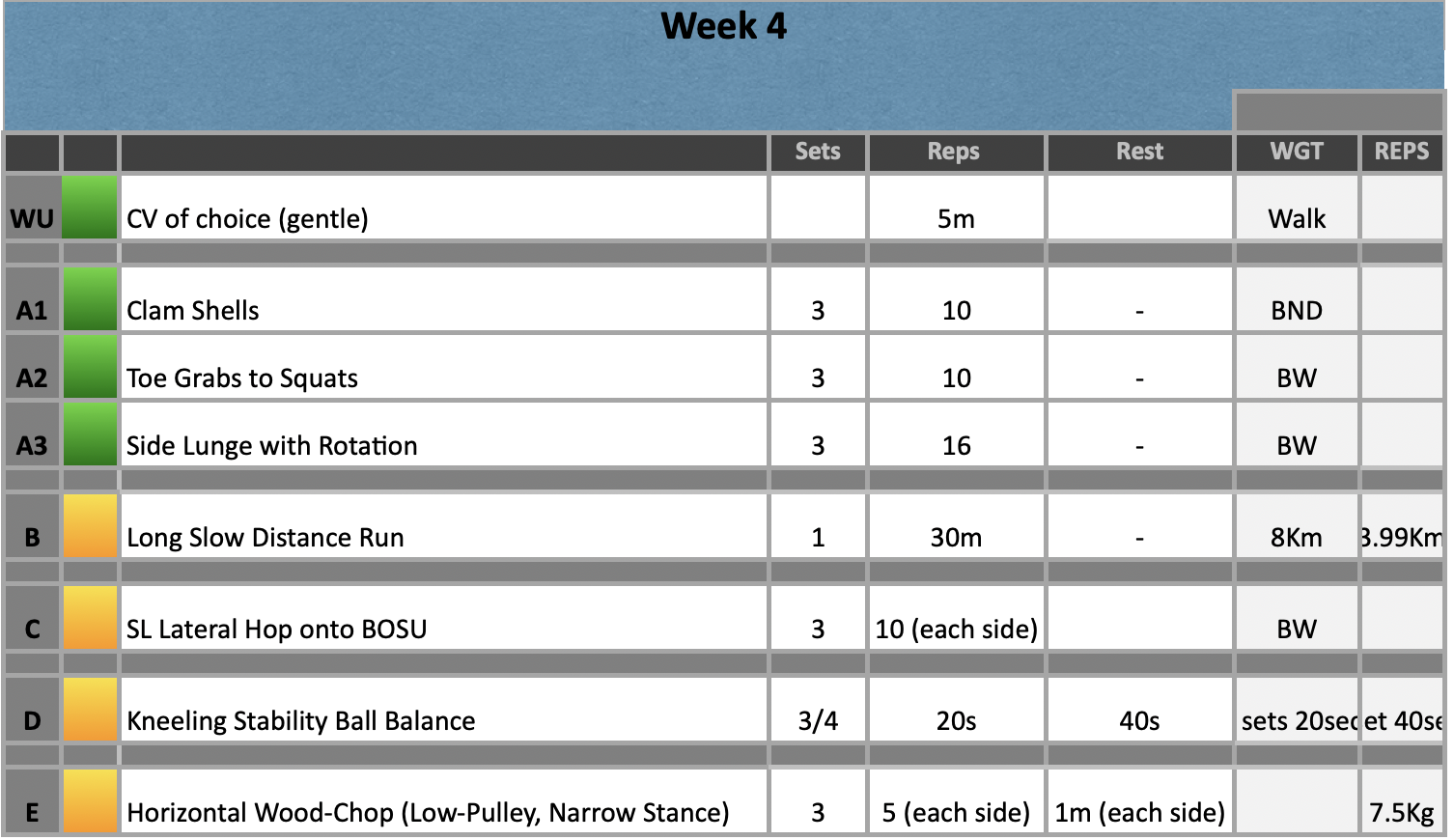
Exercise Prescription Examples
Session A
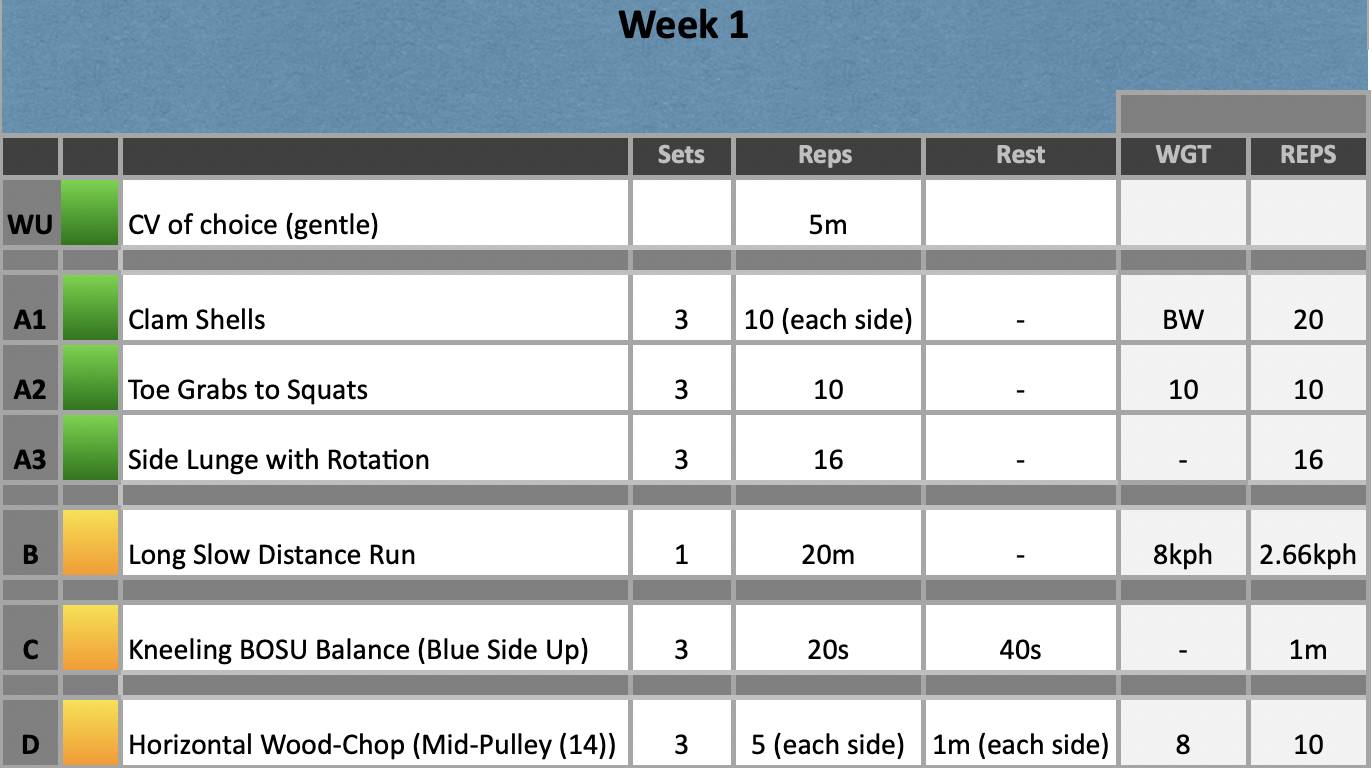
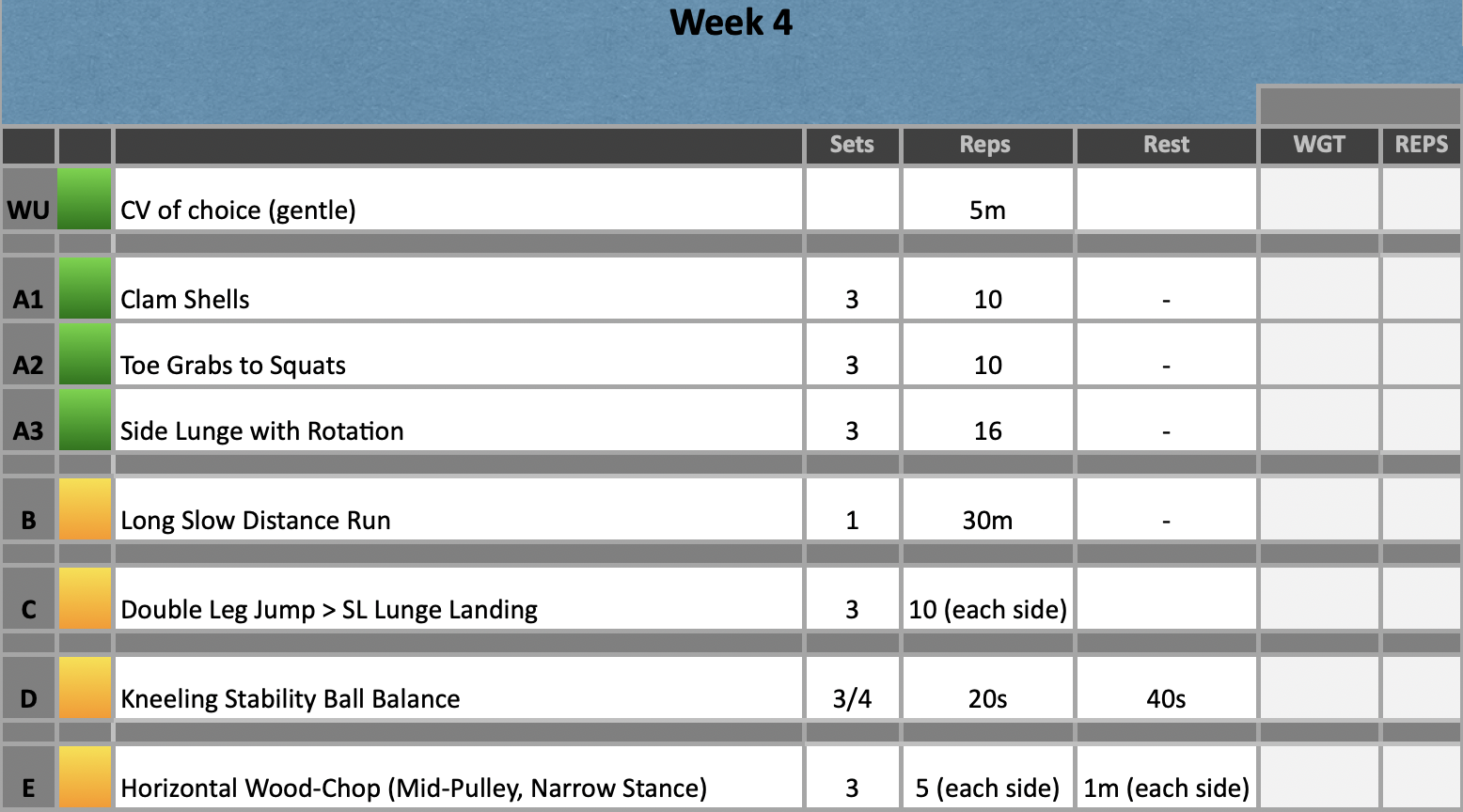
Session B
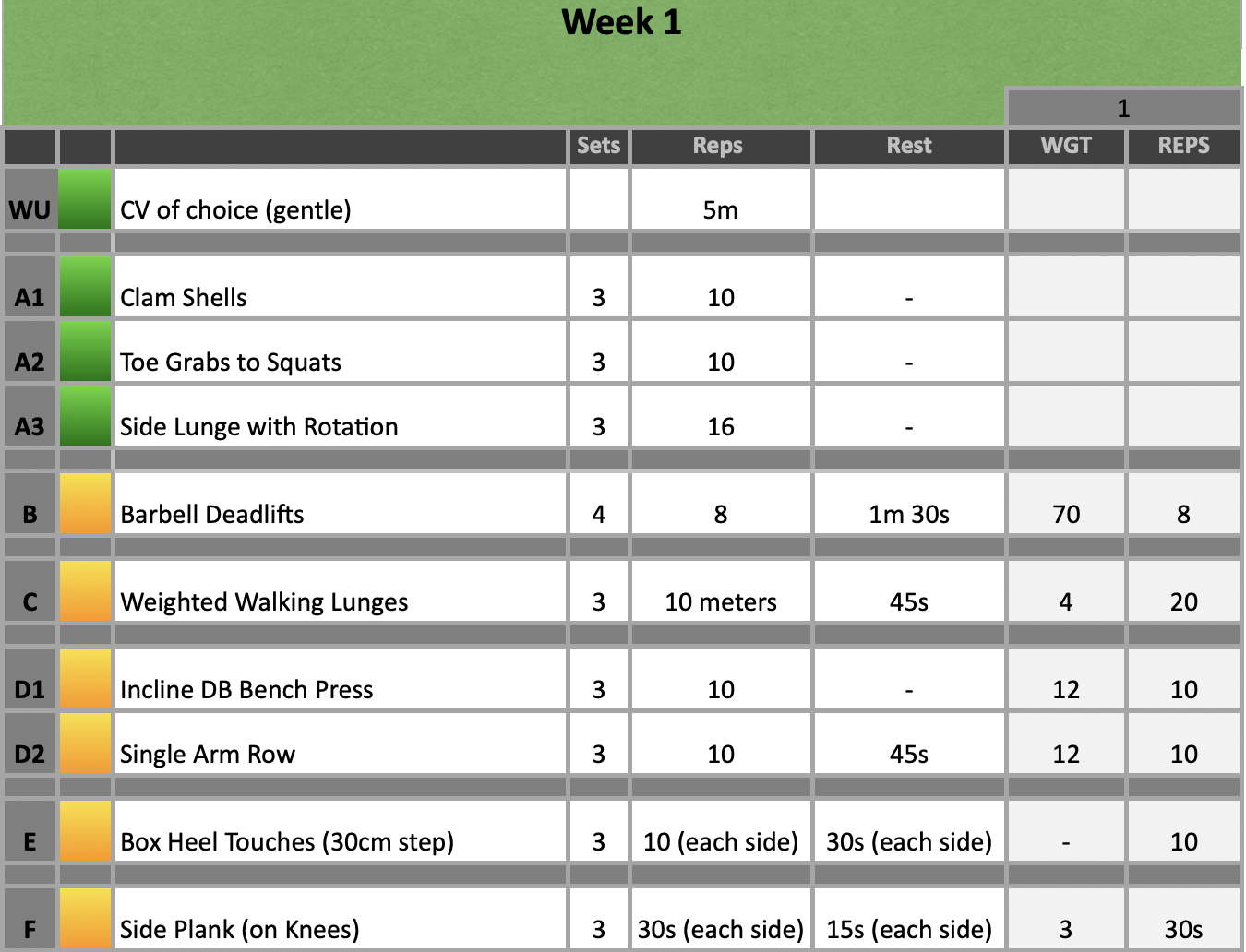
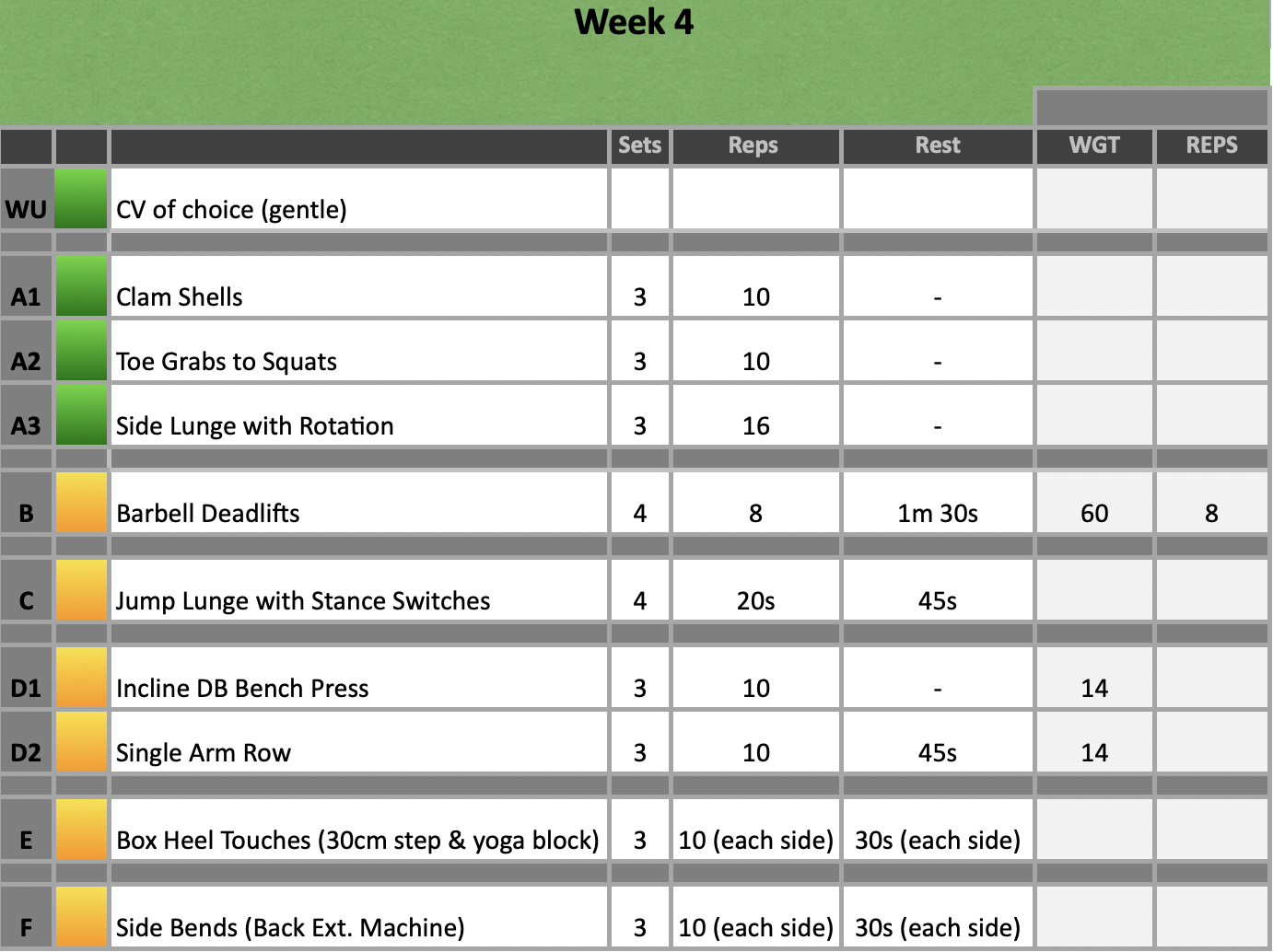
Session C

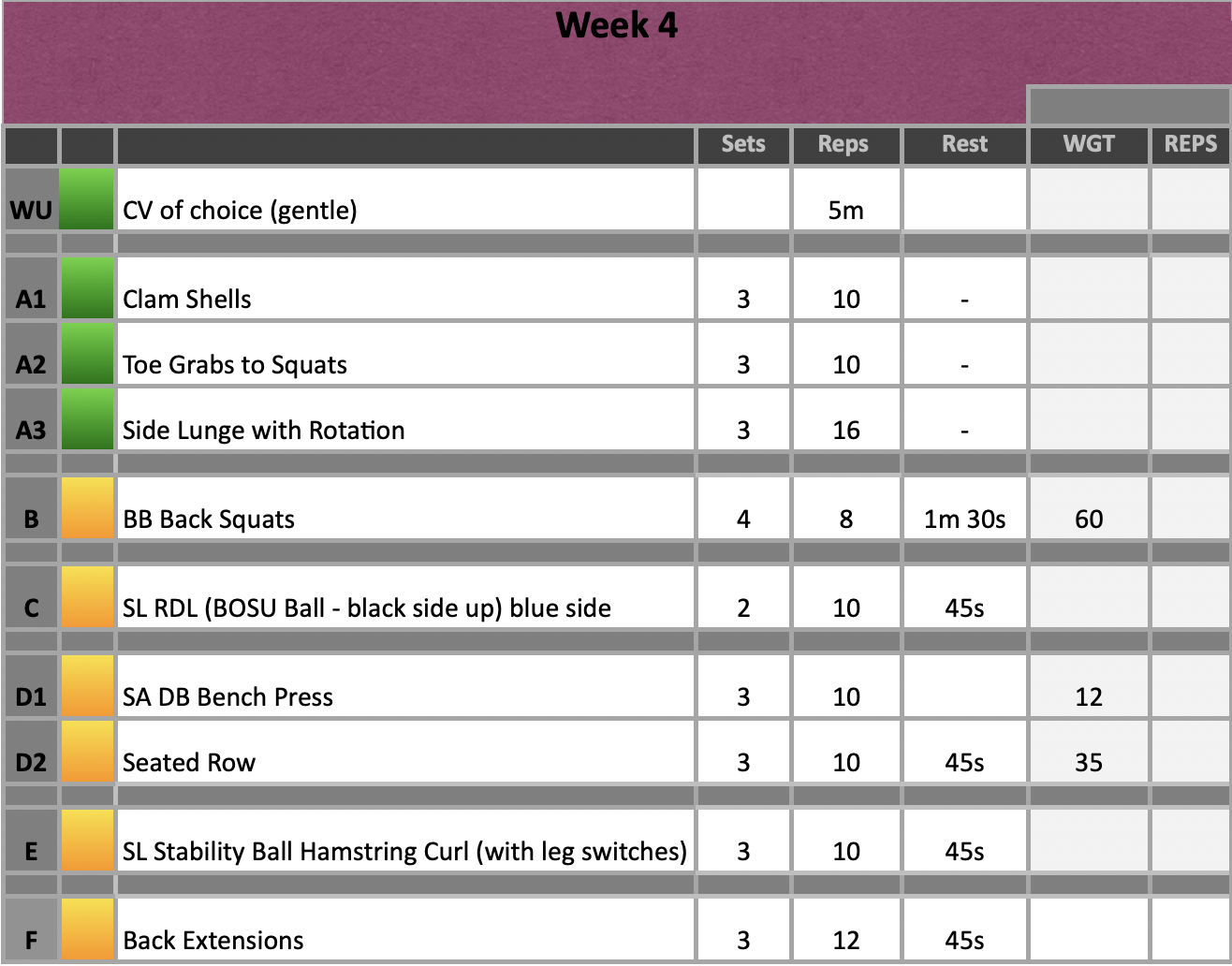
Session D
What Happened?
- Client completed a 4 week rehabilitation programme. 2 supervised sessions per week and 2 unsupervised sessions per week.
- The main goal was the correct the risky movement pattens identified during a single leg squat. Accomplishing this goal would aid in improving the dynamic stability of the knee which in turn would allow the client to progress to more challenging/high demand tasks such as COD.
- The client progressed smoothly throughout the programme. The only adjustment made was performing single leg RDL’s on the blue side of the BOSU. Initially, the plan was to progress from a yoga block to the black side of the BOSU; however, this increase in challenge was too great so we simplified the task.
- At the end of the programme the client reported no more episodes of her knee giving way and feeling like returning to hockey was actually a possibility rather than a hope.
Patient presentation Post:
- QASLS
- Affected limb 2
- Unaffected limb 0
- Quadricep LSI
- 100% with strength improvements across both limbs
- H:Q
- 90% both legs. Both limbs saw improvements in strength and both limbs were symmetrical in their strength values for both the quadriceps and hamstrings.
- ACL-RSI
- 78.3
- IKDC
- 100
What were you thinking and feeling?
- I was happy with the patient’s progress despite being nervous to take on this case. Initially, when I started reading protocols on RTP for athletes who have undergone an ACL-R, I found the sheer amount of information quite overwhelming. For example, the battery of tests used to determine RTP vary quite significantly across literature (Flagg, et al., 2019). Some advocate for quadricep LSI and others argue that is over estimates function (Wellsandt, et al., 2017). Furthermore, the accepted levels for LSI and H:Q vary significantly which made it quite challenging to decide what both myself and the client would agree is an acceptable level.
- However, as my time with the client progressed there were certain things that let me know both her knee and her confidence were improving. For example, when completing kneeling BOSU or stability ball balances the client would place herself near a walk for a safety net incase she lost balance. As the weeks progressed, she would just set up where there was available space and didn’t even think about needing a wall or any other form of external support.
What was good and bad about the experience?
- It was good to spend a significant period of time with the client and follow her journey from the start. In clinic, we are likely to get a patient who has been in before but treated by one or more therapists beforehand. This is great for honing in note-taking and note-reading skills; however, it can be unclear if your interventions or treatment were impactful or if it is an accumulation of all of them combined. Therefore, I definitely felt a sense of pride and ownership over this rehabilitation programme as I knew the results we acquired were solely from the interventions we had put in place.
- On reflection, there should have been some weeks where we didn’t look to advance the complexity of the task in order to allow the body to adjust to the new level it was required to work at. For example, we could have stuck with weighted walking lunges for a couple of weeks, maybe with some slight weight increases, before moving on to more complex movement patterns. Although, this didn’t impact the patient negatively, likely due to her significant weight training history, it is something to bear in mind if I do treat an ACL-R in the future.
Analysis
- I was actually quite surprised at the quadricep strength improvements as we only ever aimed to maintain strength due to the LSI being 100%. However, this then highlights those who are critical of LSI being an overestimation of function (Chaput, et al. 2021). Clearly, the client was displaying a symmetrical weakness across the quadriceps as opposed to an LSI that would be optimal for injury prevention. Thankfully, the programme designed targeted both quadriceps to such a degree that improvements were made across both limbs but still maintained their symmetry.
- This improvement in quadricep strength resulted in a H:Q drop; however, both hamstrings became stronger, both legs were symmetrical, and as the hamstrings are a smaller muscle group than quadriceps it is reasonable to expect hamstrings to be slightly weaker.
- QASLS was still not optimal for the affected limb; however, 4 weeks is a short time to expect neuromuscular improvements to occur (Blanchard and Glasgow, 2014). Therefore, I am hopeful that with a continuation of rehabilitation the QASLS will align with the optimal score of 0-1.
Conclusion
- Overall, I was happy with the outcomes of this rehabilitation programme. However, the clients goal is RTP and there are still some risky movement patterns to correct before returning to hockey training can commence. Furthermore, more demanding tasks such as COD, agility and plyometrics need to be mastered before RTP too.
- Therefore, I will continue working with the client on these skills until it is deemed safe for her to return to hockey.
Revisiting Reflection
- Several months after this initial rehabilitation programme, the participant strained her hamstring – the same leg which was operated on. In hindsight, I did not think about the hamstring graft that was used in her repair. Many of the exercises included, targeted the proximal hamstrings; however, I did not specifically think about incorporating distal hamstring exercises. This may have been a contributing factor to the recent injury; therefore I have made a conscious effort to target the distal hamstrings in her current rehabilitation programme, such as nordics and 1 1/2 rep RDL’s, to help protect from further injury. The client was prescribed the Askling protocol 7 days post-injury and once improvements in ROM and pain were improved we re-incorporated exercises such as deadlifts, at a lighter weight, and incorporated exercises focusing on the distal portion of the hamstrings.
References
- Wellsandt, E., Failla, M. J., & Snyder-Mackler, L. (2017). Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. The Journal of orthopaedic and sports physical therapy, 47(5), 334–338. https://doi.org/10.2519/jospt.2017.7285
- Flagg, K. Y., Karavatas, S. G., Thompson, S., Jr, & Bennett, C. (2019). Current criteria for return to play after anterior cruciate ligament reconstruction: an evidence-based literature review. Annals of translational medicine, 7(Suppl 7), S252. https://doi.org/10.21037/atm.2019.08.23
- Chaput, M., Palimenio, M., Farmer, B., Katsavelis, D., Bagwell, J. J., Turman, K. A., Wichman, C., & Grindstaff, T. L. (2021). Quadriceps strength influences patient function more than single leg forward hop during late-stage ACL rehabilitation. International Journal of Sports Physical Therapy, 16(1), 145–155. https://doi.org/10.26603/001c.18709
- Blanchard. S., & Glasgow., P. (2014). A theoretical model to describe progressions and regressions for exercise rehabilitation. Physical Therapy in Sport, 15(3), 131-135. https://doi.org/10.1016/j.ptsp.2014.05.001