Monday 12th July 2021
Hours: 4 (Observational)
Cumulative Hours: 40 (Observational)
Patient presentations:
- Knee Arthroscopy
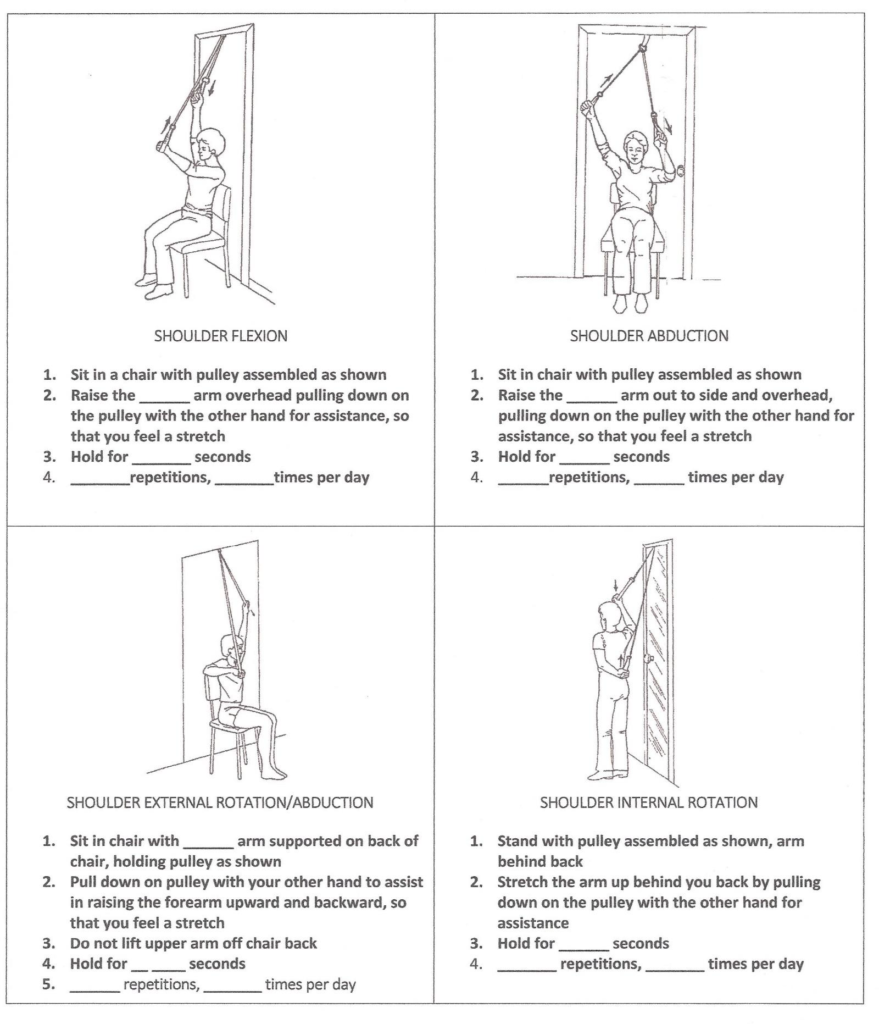
- Rotator Cuff Repair
- Knee Replacement
Reflection Focus
- Knee Arthroscopy – Plica
Reflection Model
- The ERA cycle (Jasper, 2013)
Experience
- Patient was had a knee arthroscopy 1 month ago after conservative measures failed to help with plica syndrome.
- The patient is a keen runner and was eager to try running again with permission from the physio. The session was spent in the gym and the physio guided her through some intervals on the treadmill at increasing speeds. The patient felt no pain or discomfort and the physio was happy to allow running as long as she maintained a reduced pace and shorter distances before building back up.
Reflection
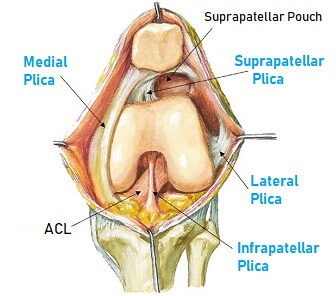
- ‘Plicae are inward folds of the synovial lining and are present in most knees.’ (Lee, 2009, p.2378). Problems arise when the structural properties of the plica change due to an inflammatory process. E.g. Over-use, particularly in activities that require repeated flexion and extension. This matches the patient history and suggests either over-training or an increase in training volume that the body could not cope with. Therefore, I am surprised there wasn’t any further education on managing her training load post-surgery.
- I was really interested in this case as I had never heard of plica before. The physio stated it is not a very well known condition and it is often misdiagnosed as other knee pathologies, such as PFPS. This thought aligns with current literature that states synovial plicae syndrome can be difficult to diagnose (Lee, 2018).
Action
- I was really surprised that there was an anatomical structure that I wasn’t even aware of. Therefore, I am going to update my anatomy notes to reflect my new learning and I am also going to add SPS to my knee injury notes with signs, symptoms and DDX.
Revisiting Reflection
References
- Lee, P., Nixion, A., Chandratreya, A., & Murray, J. M. (2017). Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain. Surgery journal (New York, N.Y.), 3(1), e9–e16. https://doi.org/10.1055/s-0037-1598047