Monday 30th August 2021 – Friday 24th August 2021
Hours: 3 (4 x 45 minute sessions over 4 weeks)
Patient presentations:
- Large mass/swelling over the greater trochanter
-
Morel-Lavallée Lesion diagnosed in August after falling from a horse onto a brick wall.
- The patient was struggling with pain over the greater trochanter and abnormal sensations in the area. The patient also has a painful shoulder just beyond 90 degrees of ABD, limited and painful IR (hand just able to reach illiac crest), painful flexion at EOR and painful ER. She was treated for whiplash by the NHS which has resolved but she suspects damage to her rotator cuff.
- Previous aspiration attempt on lesion didn’t yield much fluid and the patient is now waiting for a referral to cosmetic surgery. The area has been infected twice since the injury but currently the patient is well.
- Patient is becoming increasingly frustrated at not exercises and wants a training programme that will help with her shoulder pain and potentially her lesion. She is aware that her lesion requires surgery but doesn’t want to be sedentary in the lead up to this event
Reflection Model
- Gibbs Reflective Cycle 1988
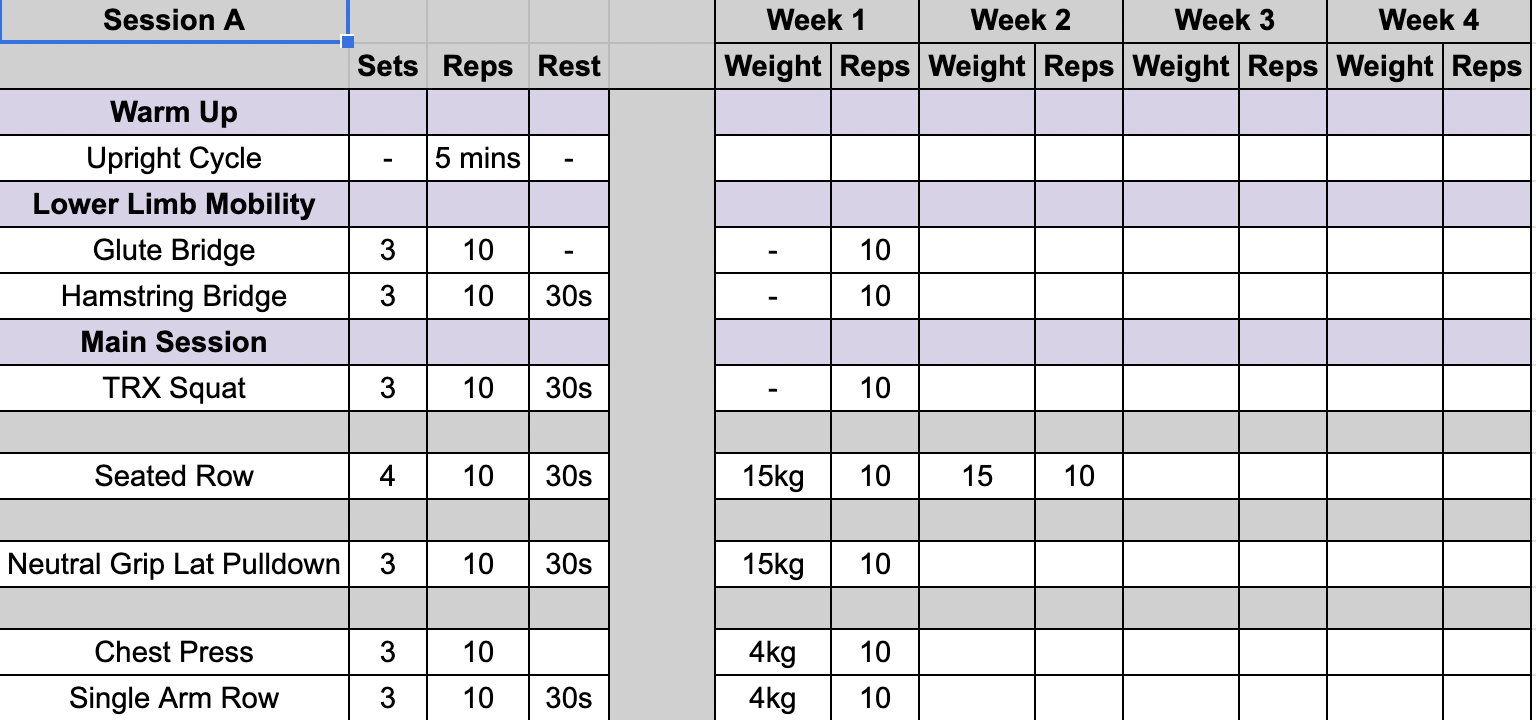
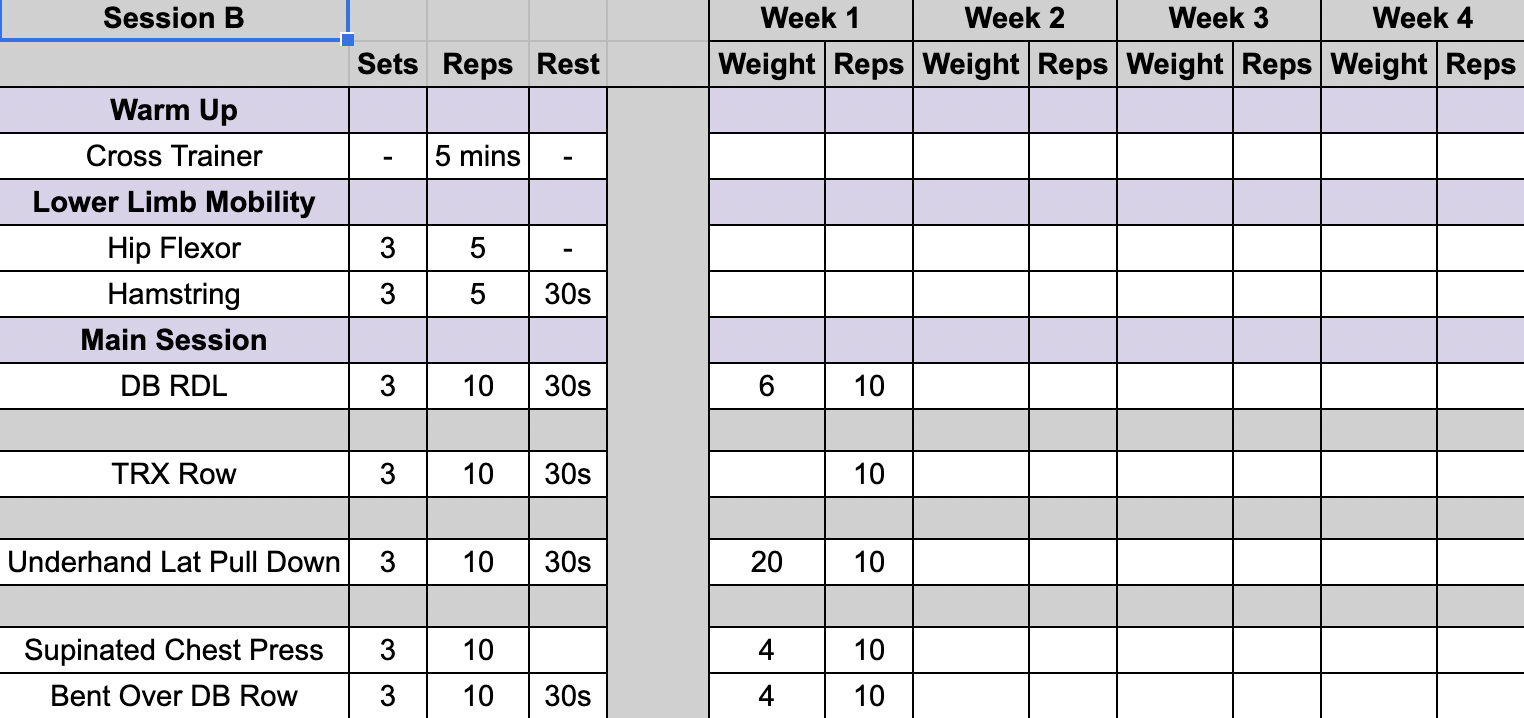
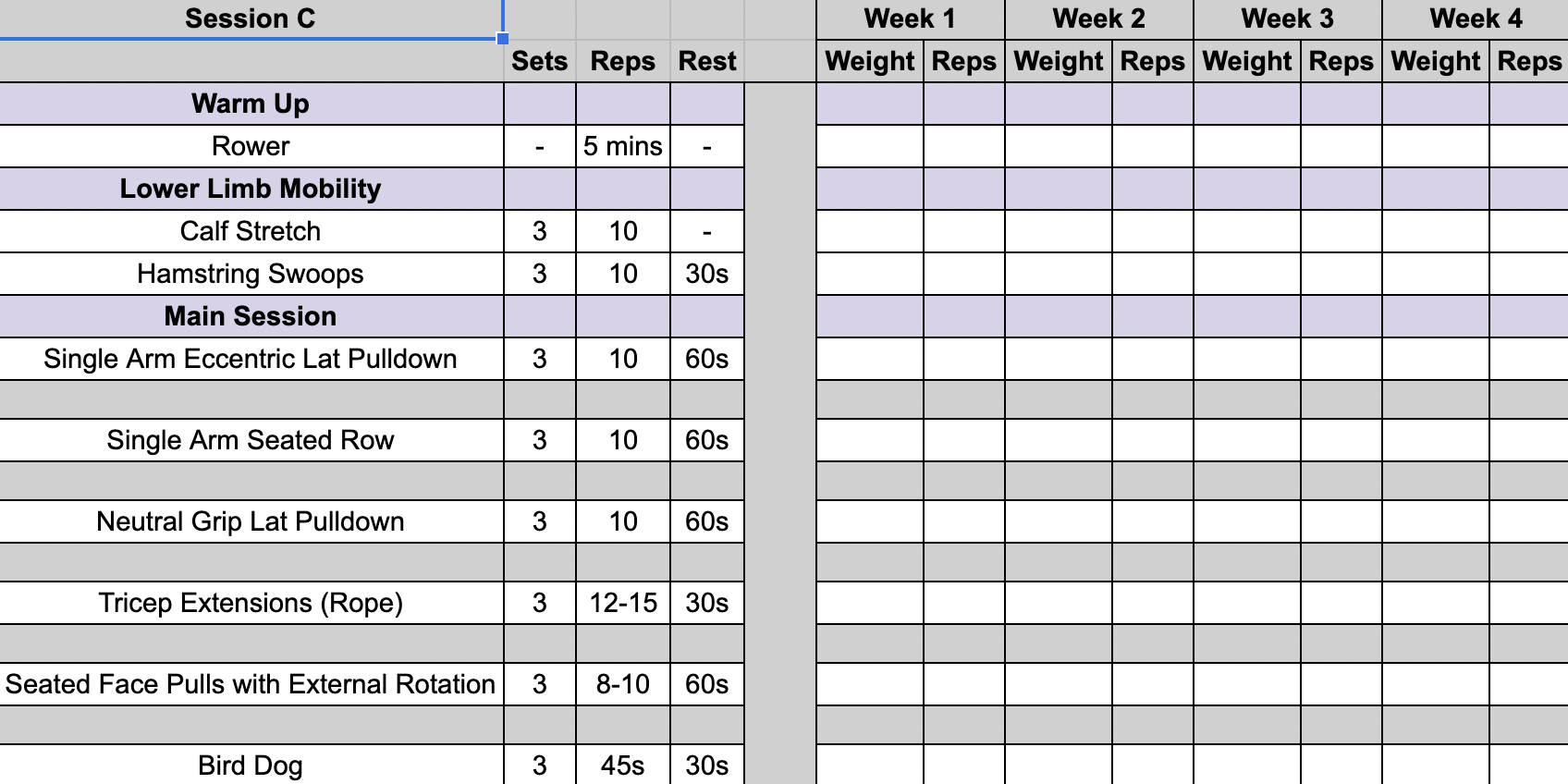
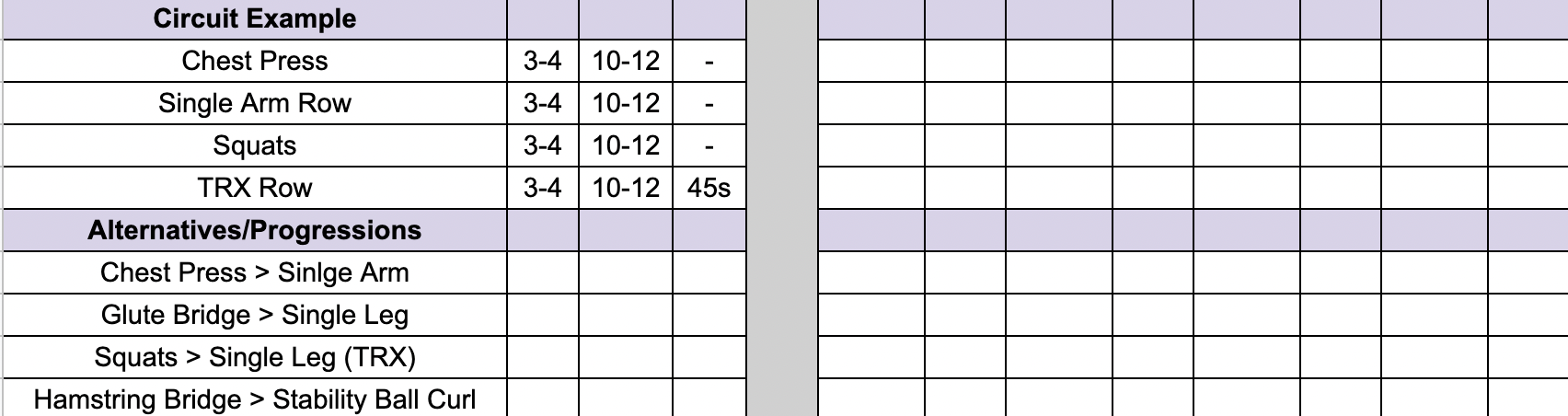
Exercise Prescription
2 unsupervised sessions per week, 1 supervised session.
What Happened?
- When the patient first saw me she had to explain the details of her diagnosis as I had never heard of it before. I asked physio’s and university tutors if they had come across this pathology before but nobody knew what it was.
- I spent a lot of time after our initial meeting, researching Morel-Lavallée Lesion. However, the literature was sparse. These lesions are common across the greater trochanter area (Miller, et al, 2014) but they can appear anywhere on the body; therefore, conservative management strategies vary. Furthermore, conservative management success depends on the severity of the injury, quick and accurate diagnosis, and if necessary aspiration (Mutuoglu, et al., 2021). There have been successful cases of conservative manage of this pathology at the knee (Doelen and Manis, 2019) and gluteal region (Harma, et al., 2004); however, the lack of an early diagnosis, excessive fluid accumulation, and lack of successful aspiration in this case indicates that surgical intervention may be the most likely resolution. Lastly, conservative management strategies appear to consist of relative rest and icing protocols rather than exercise based.
What were you thinking and feeling?
- Initally, I felt as though I should turn the patient away as there was nothing I could do for her lesion. However, she expressed that she was frustrated at being sedentary and wanted to do a little bit of exercise to keep healthy. She also wanted her shoulder pain addressed and so this was what we focused on – improving pain in shoulder and shoulder ROM.
- Light lower limb exercises were included; however, the patient knew to cease exercise if it ever resulted in a greater swelling afterwards.
What was good and bad about the experience?
- The patient had realistic expectations about her pathology and was much more interested in improving her shoulder and also psychological wellbeing.
- The patient was really good at communicating with me and she would message the next day and the day after a session to report her symptoms – even if there wasn’t anything new.
- There was a slight increase in shoulder pain during week 3 because she slept with her arm above her head. She explained that her shoulder was much better but because of this her body went back into her comfortable sleeping position. As a result, her arm was held in a position it hadn’t been in for quite some time overnight and resulted in some pain and stiffness. Myself nor the patient were concerned with this and just worked within her pain tolerance on the day she came into train.
- By the end of week 4 there was a visible reduction in her swelling; however, we never obtained an objective measure as this wasn’t something we were really focusing on. In hindsight, I should have taken a measurement to have a comparison and equally as something to monitor throughout sessions.
Analysis
- The sessions really focused on what she could do as one of the main goals was just to get her moving again despite her injuries. After looking at the Torbay Shoulder Programme we assessed ROM and pain during some of the exercises described and then adapted them to make use of the gym equipment available to us. For example, Stage 3 flexion made use of the lat pulldown, where we attached a neutral grip to perform concentric and eccentric flexion. By week 3 of the programme the client was really pleased because she was able to ‘fasten her bra and tie her hair up like a normal person.’ To me this indicated that all ROM and pain had improved to a degree that the injuries were no longer disrupting her ADL’s.
Conclusion
- Overall, the programme achieved its purpose. We didn’t aggravate the lesion and we improved shoulder function by reducing pain and improving ROM. I didn’t follow a specific protocol but my exercise selection was informed by the Torbay Shoulder Porgramme and how the patient was presenting. The patient intends to resume sessions post-surgery and maintain current exercise prescription until she is admitted for surgery.
Revisiting Reflection
References
- Miller, J., Daggett, J., Ambay, R., & Payne, W. G. (2014). Morel-lavallée lesion. Eplasty, 14, ic12.
-
Uncommon type of wound: Morel-Lavallée lesion
- Harma, A., Inan, M., & Ertem, K. (2004). Morel-Lavallée lezyonu: Kapali soyulma yaralanmalarinda konservatif yaklaşim [The Morel-Lavallée lesion: a conservative approach to closed degloving injuries]. Acta orthopaedica et traumatologica turcica, 38(4), 270–273.
- Doelen, T. V., & Manis, A. (2019). Conservative management of Morel-Lavallée lesion: a case study. The Journal of the Canadian Chiropractic Association, 63(3), 178–186.