17th January – 23rd January
- Hours: 15
Main Theme Addressed During Phone Calls
- Trying to be aware of small improvements over a larger scale of time
- 2 x discussions around returning to work
- One participant paused due an elevated RHR and BP
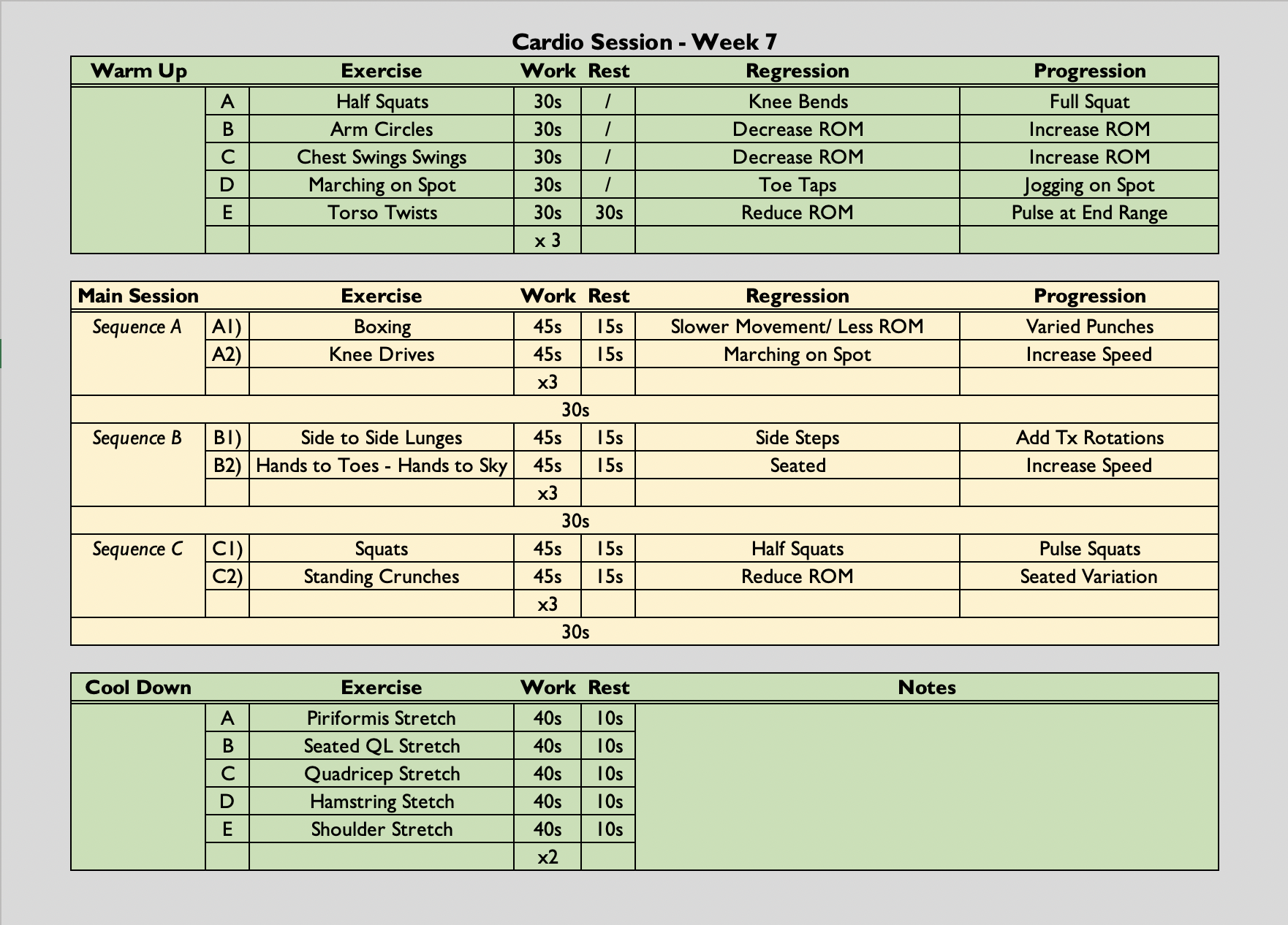
Cardio Class
- (45 secs on (90 secs if singe leg), 15 seconds off x 3, followed by a 45 second rest) x 5
- The class is always symptom-led as opposed to graded exercise therapy. Participants are free to rest when needed. They can end the class early if they have reached their limit and they can reduce the amount of sets they do if necessary.

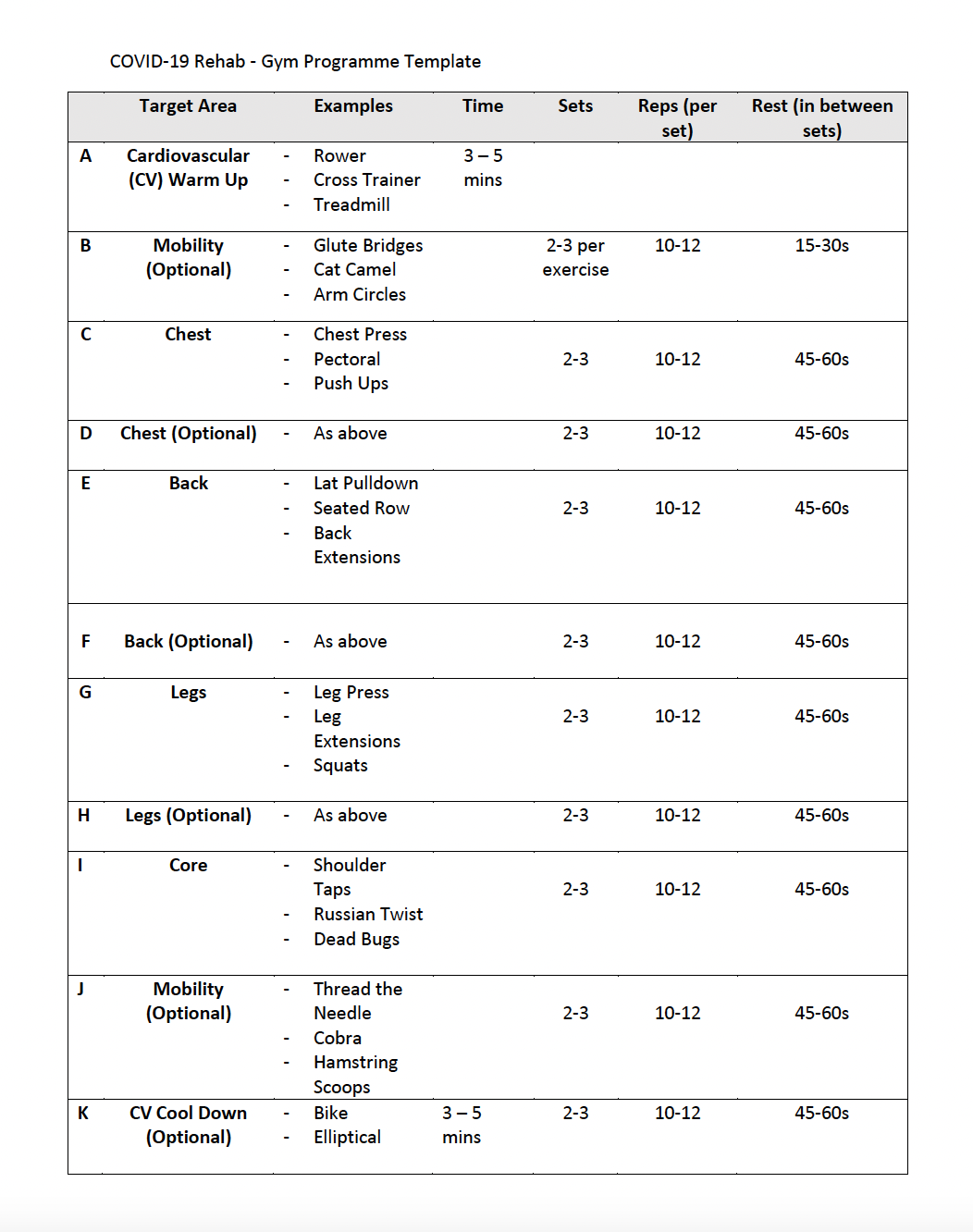
Drop-in Session
- Cohort are fairly confident in using the facilities now.
- Offered additional exercises, e.g. tricep extension using the cable machine, and variations of exercises, e.g. underhand lat pulldown as opposed to the ‘traditional’ overhand grip.
- 2 participants stay for the full 2 hours – however, they have buddied up together so have lots of rest between different exercises and have not been experiencing any negative effects post-session.
Analysis & Evaluation
- One discussion around returning to work involved the participant expressing their real want to get back to the workplace; however, occupational health and management are being very cautious and have yet to give him the go ahead. This participant notes that he is making small improvements over such an extended length of time that it is difficult to notice them. However, being able to exercise without significant exacerbations of his symptoms is a good indicator that he could start a phased return to work as previously any form of exertion resulted in excessive and debilitating proximal fatigue.
- Another discussion around this same topic involved the participant expressing the level of recovery they wish to be at before they return to work. This participant received semi-regular calls from her workplace to check-in and see how she was feeling. This participant was really firm with work and stated that she would not be returning to work until she could, on a regular basis, wake up early, do some house work, have coffee with a friend, go to the gym, make dinner and stay up until 9/10pm without, ‘feeling like the walking dead the next day.’ Her work are very supportive and as the participant is making progress agreed that all was moving in the right direction. I praised the participant for this as I have seen many participants or know many participants have returned to work far too early in their recovery. A number of people in the past have said to me, once they have taken time off work, that they feel better and will definitely go back at the end of their sick-note. I always celebrate the fact that they are feeling better with them; however, I do warn them that they may need more time before going back to work. This is because most people who are off work have the capacity to pace, plan and prioritise more effectively; therefore, their energy expenditure in comparison to a working day is markedly reduced. Rather than shift in their thinking to, ‘I know need to stabilise at baseline and then make small incremental increases to my energy expenditure overtime to prepare myself for going back to work.’ they tend to think, ‘I feel better, I should go back to work.’ The latter sees many people go back to work and struggle and/or off work again due to going back too soon. When I ask people why do they struggle through or why do they put so much pressure on themselves the answer normally falls into one of the following: guilt or financial concerns. When their reason falls into guilt I remind them that their sick-note is to declare that they are off sick from work not off sick from their life. Many people who have guilt about not being at work wouldn’t want to be seen doing what my participant described this week as they worry what people from work would say if they saw them, e.g. if she is healthy enough to go out to dinner/gym then why isn’t she at work. I try and work with these participants to challenge their thinking and put themselves first; however it can be difficult as it is a deeply rooted belief that they hold.
Conclusion
- I find it interesting that I have some people who don’t stress about not being back at work at all and others who have such an overwhelming sense of guilt who push themselves to return before they are ready. From this experience, I am going to explore any evidence that might exist on returning to work after a period of absence and what psycho-social factors play a role in this decision.
Revisiting Reflection
- On further investigation, I found the NHS offers guidance and support about returning to work – therefore, I will ensure I offer this to participants who may be struggling alongside advise of planning, pacing and prioritising.
- I found that the UK Government has acknowledged that psychosocial factors may impede an employees return to work. Fear of social stigmatisation, anxiety, depression and PTSD are quite common in those living with long covid. Therefore, it has been suggested that returning to work and moderate physical activity could be beneficial to those who have poor mental wellbeing. In terms of returning to work, it has been suggested that the employee have more control over the situation to reduce psychological distress or symptoms. I think in the future it would be beneficial to share this information with participants as some feel like have no say or guidance in their phased return process.