Tuesday 26th Ocotober 2021
Hours: 3
Patient presentations:
- Therapeutic US
- Oblique Strain
- LBP after n0n-contact trauma
Reflection Focus
Reflection Model
What Happened?
- A very brief treatment as the patient needed to have a COVID test before commencing training for the day.
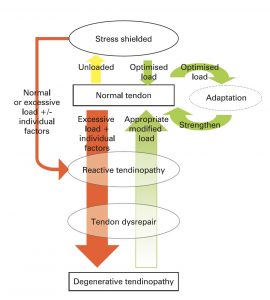
- Presenting with reactive achilles tendinopathy. Patient had previously received general maintenance on calves through STM, mobility and stretching exercises. Today he was in for another session of Therapeutic US.
- 3Hz, 100%, 6 minutes.
What were you thinking and feeling?
- Within in clinic, I have many patients who have seen a previous therapist for their current injury. However, this was the first professional sports person I had treated which means not only were there recommendations from the previous therapist but the patient would also be receiving guidance and information from multiple different coaches.
- As this was not a day I would normally be in clinic I decided to abide by the previous therapists notes and follow the course of treatment they had planned.
What was good and bad about the experience?
- I think I made the right decision not to offer any further advice/information as it may have resulted in information overload or even confused the patient if it conflicted with previous recommendations. However, I did reiterate that the stretching and mobility he had been prescribed previously was an important factor in his recovery. This was to ensure that he considered his exercise prescription as something as equally important as the passive treatments he was receiving.
Analysis
- On reflection, I should have queried the Ultrasound settings used previously. As a lower pulse dose may have been enough e.g. 1:2, as the condition was only just moving into the subacute stage (Watson, 2017). However, the patient did report that his Achilles had been feeling better since his last treatment; therefore, I didn’t want to make changes to his treatment plan that may have been having a positive effect. Equally a study by Chang, et al., 2015 delivered therapeutic ultrasound in continuous mode for 8 mins on the achilles tendon and it resulted in increased tendon microcirculation via an increase in vasodilation. Vasodilation will optimise blood flow, cell permeability and nutrient delivery at the injured site, thus improving the quality and potentially rate of injury resolution.
Conclusion
- I learned that it is not only important to reflect on my own treatment plans but also pre-existing treatment plans not initiated by myself. If I had seen this patient from the on-set I would have likely delivered ultrasound on a pulsed dose (1:2), which may not have been as effective as reducing the patients pain. I can’t say this with certainty as there were other contributing factors such as a mobility and stretching routine that the patient was following. I think overall I made the right decision in following the treatment plan and not changing the does; however, if the patient presented differently, e.g. worsening or static pain, I would have used a different dosage as the tissue may have been too sensitive to the continuous mode of delivery.
Revisiting Reflection
References
- Chang, Y. P., Chiang, H., Shih, K. S., Ma, H. L., Lin, L. C., Hsu, W. L., Huang, Y. C., & Wang, H. K. (2015). Effects of Therapeutic Physical Agents on Achilles Tendon Microcirculation. The Journal of orthopaedic and sports physical therapy, 45(7), 563–569. https://doi.org/10.2519/jospt.2015.5681