Monday 16th August 2021
Hours: 5
Patient presentations:
- 8 months post lateral ankle sprain
- Piriformis Syndrome/Discogenic Pathology
- Anterior knee pain & bilateral groin related hip pain.
- Suspected MCL sprain/Meniscal tear.
Reflection Focus
- Suspected MCL sprain/Meniscal tear.
Reflection Model
- Gibbs Reflective Cycle 1988
What Happened?
- Patient’s 3rd appointment. Complaining of knee pain, crepitus and locking after a hit to the knee during a rugby game. In previous weeks the clinic generated a referral letter for the patients GP to book an MRI.
- The patient’s day-to-day pain has reduced and periods of locking have become less frequent.
- The patient has family visiting at the end of next month and they want to watch him play a game of rugby. The patient wanted to know if he would be able to play by the end of September.
What were you thinking and feeling?
- I was particularly concerned that this patient had become disengaged with his rehabilitation. He asked if there was any point in doing the exercises until he had his MRI. Furthermore, despite reporting that running didn’t feel normal and having no explosive movement on the affected limb he was still participating in high demand training drills, such as suicides.
- I did feel empathetic towards this patient as it was clear that his family coming to watch him play meant a lot to him. However, the patient was 18 years old and with his knee still far from what he would deem normal I didn’t want to risk him playing and sustaining further damage to his knee.
What was good and bad about the experience?
- I felt like I explained my concerns regarding the patients engagement with the rehabilitation process well. I was clear that the MRI may not indicate surgical intervention and that conservative management may be advised; therefore, continuing would keep him on track towards recovery (Mina., et al. 2015.) I also iterated that even if the MRI did indicate the need for surgery the outcome from this would likely be better if he engages with prehab.
- I also involved the patient in a discussion about life outside of rugby. The patient noted that if he played in September and was injured further this would impact the progress he is making on his driving lessons. At this point of the assessment, I felt that the patient was starting to understand the wider implications of playing on an injury.
Analysis
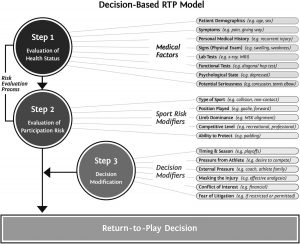
- I think discussing the wider implications of returning to play was important in this situation. I would not have felt comfortable advising the patient that it was safe to play given his injury and I was loosely following the StaRRT Framework to inform this decision. (Shrier, 2015.) I believed that the patient’s tissue health was not strong enough to withstand the stresses that would be placed on it during a game of rugby, especially as he would likely want to perform at 100% for his family who would be watching. Furthermore, considering the patients desire to continue playing rugby and progress to increasingly higher competitive levels the overall risk of playing seemed too great.
Conclusion
- Overall, I think I handled the RTP question well but I think we didn’t handle the topic of a referral particularly well with the patient.
- In the future, if a situation like this presented itself to me, I would make it clear from the very beginning what a referral for imaging entails and what the patient’s best steps are moving forward. It is possible that by generating a referral, and not explaining what this meant in any great detail at the time, the patient thought we couldn’t offer him any further help.
Revisiting Reflection
References
- Mina, D., Scheede-Bergdhal, C., Gillis, C & Carli, F. (2015.) Optimization of Surgical Outcomes with Prehabilitation. Applied Physiology, Nutrition and Metabolism.