24th January – 30th January
- Hours: 15
Main Theme Addressed During Phone Calls
- 2 participants starting to feel like themselves anymore and rarely think about long-covid
- 1 participant opened up to have been dealing with a breast cancer scare since Christmas.
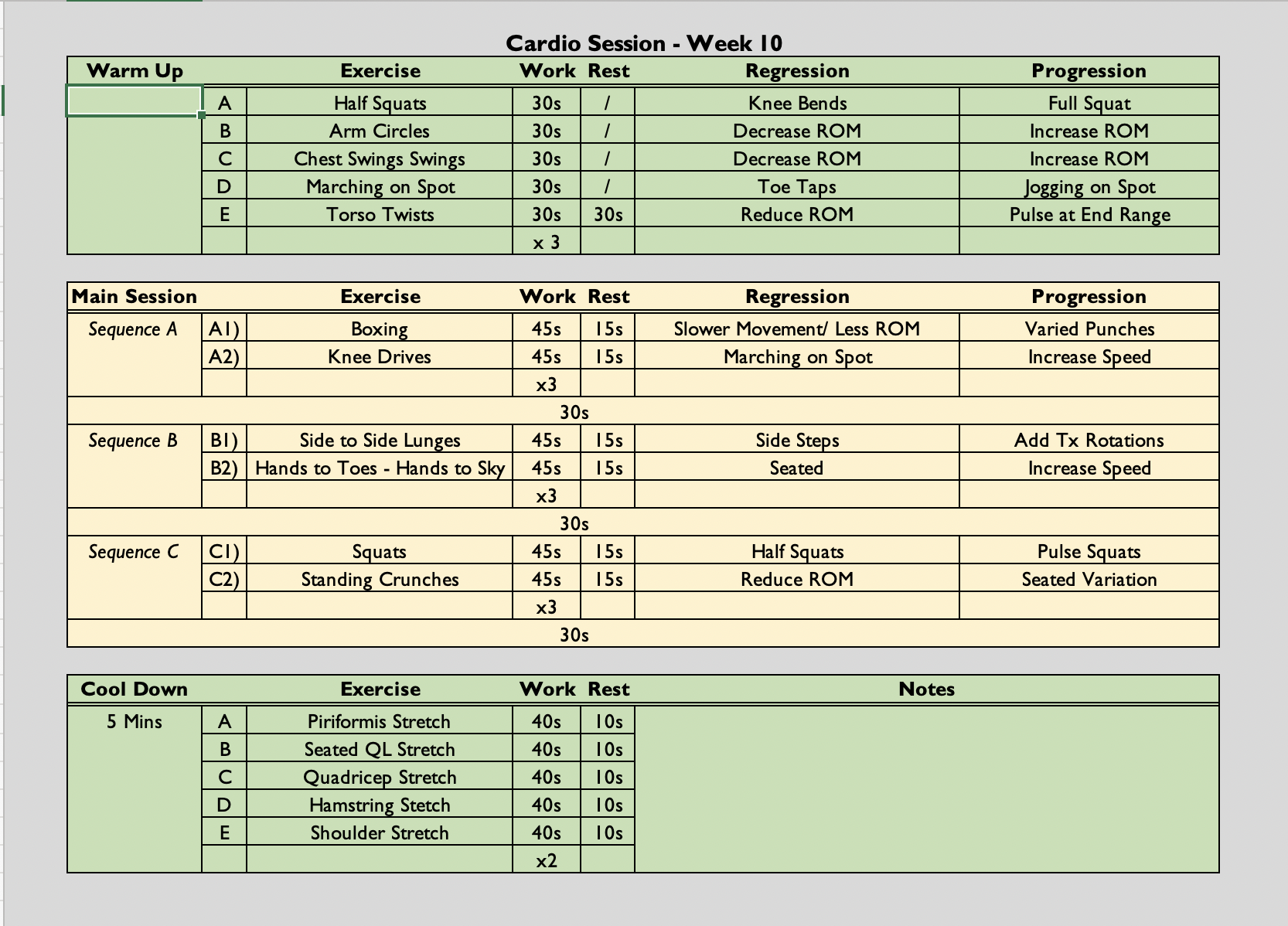
Cardio Class
- ((45s secs x 2 followed by a 30 second rest) x 3) x 3
- The class is always symptom-led as opposed to graded exercise therapy. Participants are free to rest when needed. They can end the class early if they have reached their limit and they can reduce the amount of sets they do if necessary.
Analysis & Evaluation
- Interestingly, two of the participants who have started to feel much better as the two participants whose attendance is a bit up and down. One more so than the other but attendance isn’t what it once was. As they both started to report in phone calls that they started to feel better other things started to take priority, e.g. taking kids to a football match or taking the kids to football.
- I found myself really conflicted with both these participants as I felt I needed to encourage them to maintain their rehabilitation in order to ensure they were stable. I didn’t want either of them to do too much one day and then experience a relapse. However, the things they were doing instead of the programme were elements of their life that they missed due to their long covid so, I felt their progress needed to be celebrated.
- We have been taught that rehabilitation should be patient-centred and fit the patient’s lifestyle. And, unlike many sports injury, there isn’t a set protocol on how to successfully rehabilitate people living with long COVID. As the activities that these participants were doing, required an energy expenditure that they were not capable of before then there is no reason for me to assume that ‘unstructured’ exercise doesn’t hold a place in their rehabilitation. Especially, when I consider the psycho-social impact COVID can have on participants. It is worth noting that limited social support or family support has been shown to be a barrier to adherence (Jack, et al., 2010); however, in this instance it seemed actually having that support hindered their adherence. Both of these participants reported extremely supportive families and that they wanted to get back to feeling normal with them again.
- Another participant this week opened up about a breast cancer scare she has been dealing with since Christmas. She initially told me via email and we then discussed how she was at her weekly 1-1 phone call. Naturally, the scare had been weighing on her mind – her biopsy was coming up soon and she was dreading the thought of having to deal with cancer on top of her long covid. I just listened to what the participant had to say and refrained from offering advice in this situation. During our EWB training, when dealing with significant EWB concerns that are beyond our scope of practice we are to practice repeat back what the participant has said, thanking them for sharing the information and asking questions such as, ‘ is there anything you would like me to do know that you have shared this with me?’ The participant confirmed that she just wanted to keep me informed and that she would need a some time off from exercise as he biopsy fell the day before an exercise class. This particular participant has reported no improvements in her fatigue since starting the programme. However, she has also been quick to reject any possibility of time off work or trying to slow down. So, I did wonder if since the scare started if she has been trying to keep herself busy so she would be distracted and maybe not think about it as much. Situations like this, highlight that rehabilitation needs to be flexible when it is called for. Many participants worry that if they don’t attend for whatever reason that we would remove the from the programme. However, as this situation and also the previous two highlight, there are many reasons to justify non-attendance. I think the important thing is ensuring that attendance doesn’t start to diminish entirely.
Conclusion
- I have always assumed that people don’t adhere to rehabilitation because they don’t understand why it is relevant to them, they find it boring or they don’t see results quickly enough. However, adherence is much more nuances than that. This week has shown me that actually non-adherence may be a sign of successful rehabilitation that requires further progression or it may be a sign of more complex matters at hand that need to be addressed above their current rehabilitation programme. I think the challenge then lies in having these participants return to the programme on a consistent basis. Non-adherence, although not ideal, is sometimes not avoidable; however, it is important to get people back on track once this has happened and have a shared discussion about how this may look for them going forwards.
Revisiting Reflection
- Jack, K., McLean, S. M., Moffett, J. K., & Gardiner, E. (2010). Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Manual therapy, 15(3), 220–228. https://doi.org/10.1016/j.math.2009.12.004