Me and another sports therapist provided post-match treatment to the BUCs hockey players, if they requested it. The majority of treatments consisted of soft tissue massage (STM) and METs (Muscular Energy Techniques).
| Reflective Summary
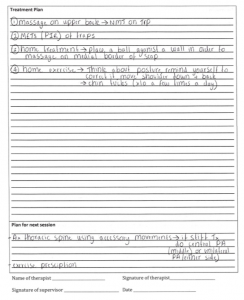
Before beginning the treatments, I check THREADS and contraindications, specifically asking the client if they were allergic to any of the massage mediums and if they preferred the use of a particular one. Client 1: The first client requested soft tissue therapy on the calves, hamstrings and lower back. I started with the calves and then worked up. Throughout I used the correct towelling technique to ensure client modesty. As there were two sports therapists present for this treatment, we could each massage one side of the body. I used effleurage to stimulate the flow of lymph fluid that leads to increased drainage of waste products, as well as inducing relaxation and reducing abnormal muscle contraction (Keperawatan, Petpichetchian, & Chongchareon, 2013). I also used a lot of petrissage including kneading and wringing to increase the blood flow, in order to transport more oxygen and nutrients to the tissues and remove waste products, promoting an efficient system (Findlay, 2018). Client 2 (see appendix): The next client explained that they have irritation around the medial border of the scapular and the pain experienced is a dull ache. The player explained that they consistently stretch pre and post training and have tried various treatment methods to try and decrease the pain including ultrasound and soft tissue massage. The most pain-relieving technique for her was neuromuscular technique (NMT) so I combined this with massage and used METs to improve musculoskeletal function, pain relief and increase range of motion (ROM) (Dhinkaran, Sareen, & Arora, 2011). I used METs of the upper trapezius, specifically post isometric relaxation (PIR) as it is more effective then reciprocal inhibition (RI). This is because the contraction of the affected target muscle group (PIR) was not uncomfortable or aggravating (Ward, Di leva, Thain, & Gardiner, 2015). Client 3: The final player also had a lot of trigger points underneath the scapular from both CrossFit and hockey. During the assessment the tighter side was her non-dominant side. She explained she use to carry her children on this side, so this could be linked to the increased tightness. Soft tissue therapy was used to relax and reduce abnormal muscle contraction therefore decreasing muscle tightness (Keperawatan, Petpichetchian, & Chongchareon, 2013). Areas for further improvement My first area for further improvement would be to reference outcome measures such as the client’s range of motion (ROM) passively, strength using the oxford scale and pain (VAS pain scale). This is important to do as it helps to gauge if methods chosen were beneficial to the client. Another thing I need to do to further my learning would be to research and look at the literature surrounding trigger points, in and around the medial border of the scapula and the most effective treatment for it. Many people experience tightness around this area and learn to live with it but as part of my profession, we want to find the most appropriate way to both prevent and treat it. Finally, I always need to consider the use of other treatment modalities/methods, not just soft tissue massage. This is because some methods may be more effective for a specific aim. Things to Remember:
References Dhinkaran, M., Sareen, A., & Arora, T. (2011). Comparative analysis of muscle energy technique and conventional physiotherapy in treatment of sacroiliac joint dysfunction. Indian Journal of Physiotherapy and Occupational Therapy, 5, 127-30. Keperawatan, C., Petpichetchian, W., & Chongchareon, W. (2013). Does Foot Massage Relieve Acute Postoperative Pain? A Literature Review. Nurse Media Journal of Nursing, 3(1), 483-497. Ward, K., Di leva, R., Thain, P., & Gardiner, N. (2015). Clinical Interventions in Sports Therapy.Abingdon-on-Thames: Routledge. Appendix Clinical consultation form: |