29th November – 5th December
- Hours: 15
Main Theme Addressed During Phone Calls
- Emotional Wellbeing (EWB) and its impact on recovery
- A number of patients reported a sense of worry and anxiety post-covid. For example, ‘how will I earn money if I am off work?’ ‘I don’t look sick so people will think I am lazy if I say no to things.’ During the phone calls I iterated that it is normal to experience worry and anxiety; however, when it becomes all-consuming or intrusive then this is something that needs to be addressed. I iterated that worrying will contribute to fatigue, particularly brain fog , as the mind is constantly wired. I didn’t actually give this advice based on evidence it just, at the time, felt like a caring but logical piece of information to highlight.
- However, afterwards I paused to reflect. Many of the patients I have worked with have previously been given advise from GP’s to manage their condition as though they have chronic fatigue syndrome (CFS). Literature has also made links between long covid and CFS for example, a review by Wong and Weitzer highlighted the similarity of both CFS and long covid symptoms (2021). And, there is evidence that links neuroticism and maladaptive perfectionism to fatigue and/or CFS ( 2010; Valero. et al., 2013). Therefore, helping to manage levels of worry, anxiety and internal pressures patients may place on themselves may be a crucial aspect of their rehabilitation.
- A number of patients reported a sense of worry and anxiety post-covid. For example, ‘how will I earn money if I am off work?’ ‘I don’t look sick so people will think I am lazy if I say no to things.’ During the phone calls I iterated that it is normal to experience worry and anxiety; however, when it becomes all-consuming or intrusive then this is something that needs to be addressed. I iterated that worrying will contribute to fatigue, particularly brain fog , as the mind is constantly wired. I didn’t actually give this advice based on evidence it just, at the time, felt like a caring but logical piece of information to highlight.
Case Study for MDT meeting Tuesday 7th December
- This week. I also gathered information on a particular case to present for the MDT as I was looking for further guidance on appropriate management.
- The participants main complaint = Proximal Weakness (Shoulders and Thighs).
- Symptoms = Extreme fatigue in shoulders after ADL’s, such as brushing teeth, combing hair, typing, writing, driving, and eating. Walking any incline was once difficult but there has been some improvement. Fasciculations in thighs are not as frequent as they were in early recovery, but he may still experience them after exercise.
- Impact = The patient returned to work after COVID-19; however, 5-6 months ago his shoulders deteriorated to such a degree that he could no longer work. The patient is a doctor at the local hospital. His shoulders have not improved since the deterioration.
- Medical Interventions = Blood tests, nerve conduction studies and an EMG. All results were normal.
- Pattern = After a night’s rest both shoulders and thighs feel completely normal. However, as soon as he does something minimal, such as brush his teeth, he feels the fatigue in his shoulders. If he pushes them too far, e.g., a long drive, the fatigue he feels will not resolve unless he rests for an extended period, e.g., a night’s sleep.
- Currently on Week 2 of the programme. Each exercise session to date has made him ‘more aware of fatigue than usual’ the next day. However, after 2 days he returns to his current baseline. Rated week 1 cardio class 9/10 in terms of muscular fatigue and he struggled to perform the shoulder stretch during the cool down.
- Management suggestions from MDT:
- Focus on improving grip strength as an indirect shoulder strengthening exercise.
- Closely monitor for signs and symptoms of PoTS. Consider measuring SpO2 whilst exercising.
- Discussion was had around coat hanger syndrome; however, the patient does not experience any pain and this would not explain the weakness in the thighs.
- I initially thought the participant was presenting with polymyositis; however, this would have been ruled out with his blood tests and EMG. The conclusion from this meeting was to continue managing symptoms and monitor closely for any deterioration. My current line of thinking is to work on strengthening all the surrounding musculature e.g. triceps, biceps, glutes and calves. If they are able to get stronger they may offload the shoulders and thighs and provide some relief to the participant.
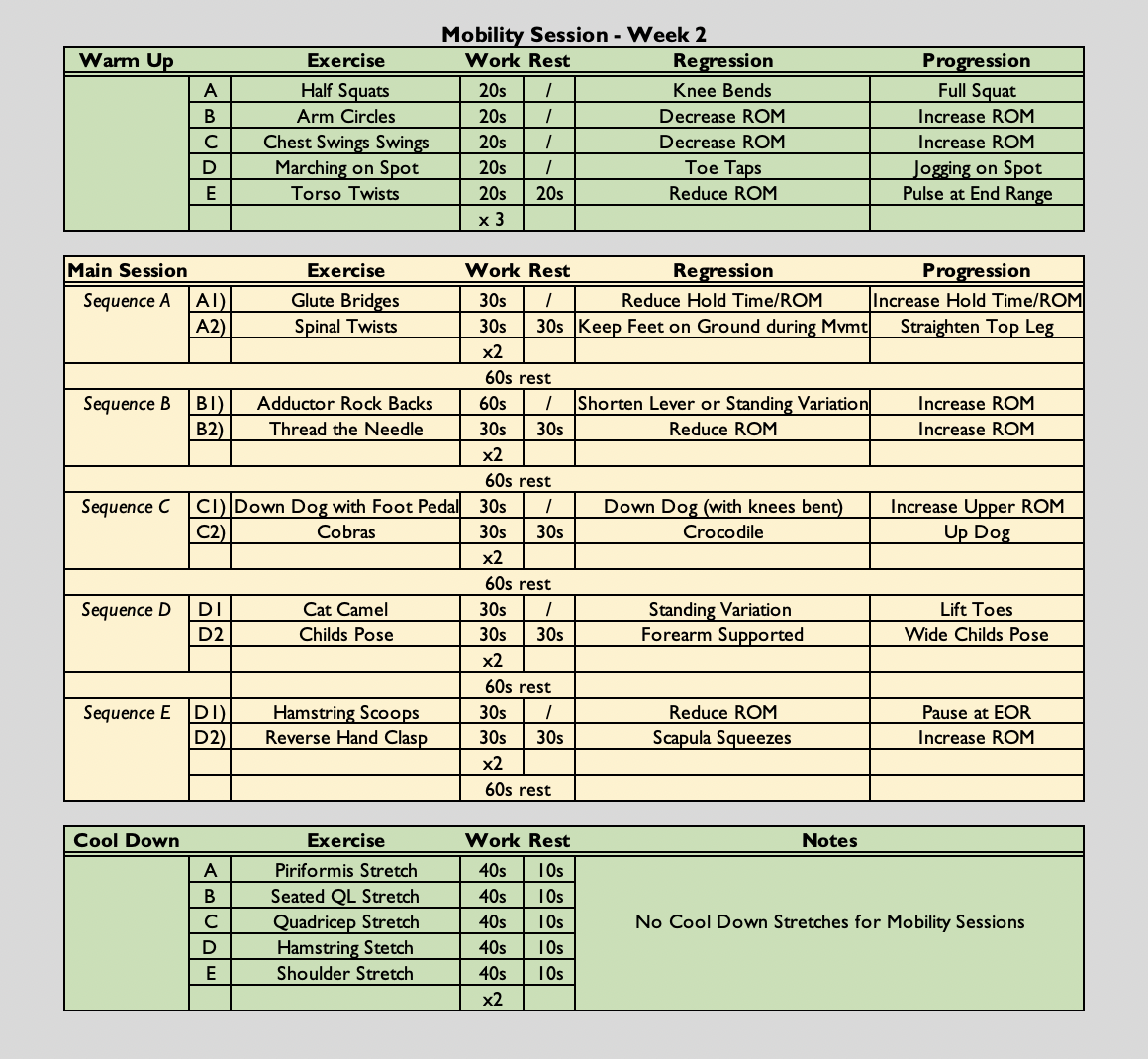
Mobility Class
- (6o secs on, 30 seconds off (2:1) x 2, followed by a 60 second rest) x 5
- The class is always symptom-led as opposed to graded exercise therapy. Participants are free to rest when needed. They can end the class early if they have reached their limit and they can reduce the amount of sets they do if necessary.
Analysis & Evaluation
- I felt I provided suitable advice this week, particularly around the topic of worrying. However, I feel that this is an area I could improve on further and find some additional strategies for patients to utilise. Currently, I advise patients to reflect on unhelpful thinking and identify ways they could change their thinking to be more helpful. For example, rather than ‘I can’t do this – I will never be normal again’ try ‘Recovery takes time and I am making small improvements that show my body is healing itself. I also advised them on creating a time and space for worry so it does not interfere with their day; however, many struggle with being able to compartmentalise in this way.
- It wasn’t great that the MDT meeting didn’t provide any clear cut answers. However, it is good to know that my current approach is acceptable and I haven’t missed any red flags
Conclusion
- Currently the exercise class is still virtual; however, when the course transitions to an in-person setting I will provide exercises to the participant struggling with proximal weakness as mentioned previously to see if this makes a difference.
- Furthermore, it may be helpful to have more tools at my disposal to help those with worry and anxiety. I may need to accept that an onward referral is required as their needs may be more complex than the support I can offer. However; waiting lists and accessibility can be an issue for EWB services, so it is important that I can offer some strategies in the interim or at least signpost individuals who could benefit from some extra help and support.
Revisiting Reflection
References
- Wong, T. L., & Weitzer, D. J. (2021). Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)-A Systemic Review and Comparison of Clinical Presentation and Symptomatology. Medicina (Kaunas, Lithuania), 57(5), 418. https://doi.org/10.3390/medicina57050418
- (2010). Personality and perfectionism in chronic fatigue syndrome: A closer look, Psychology & Health, 25:4, 465-475, DOI: 10.1080/08870440802403863
-
Valero, S., Sáez-Francàs, N., Calvo, N., Alegre, J., & Casas, M. (2013). The role of neuroticism, perfectionism and depression in chronic fatigue syndrome. A structural equation modeling approach. Comprehensive psychiatry, 54 7, 1061-7 .